Foot pain top of foot is that sharp, annoying ache that starts as a whisper after a long Sunday run and before long is loud enough to ruin a session. If it’s happening to you—especially while training for the Sydney Marathon, Gold Coast Marathon or Ironman Cairns—this practical, coach-first guide shows exactly what to test, how to treat it, and the training adjustments to stop it from coming back.
So, what’s really going on up there?
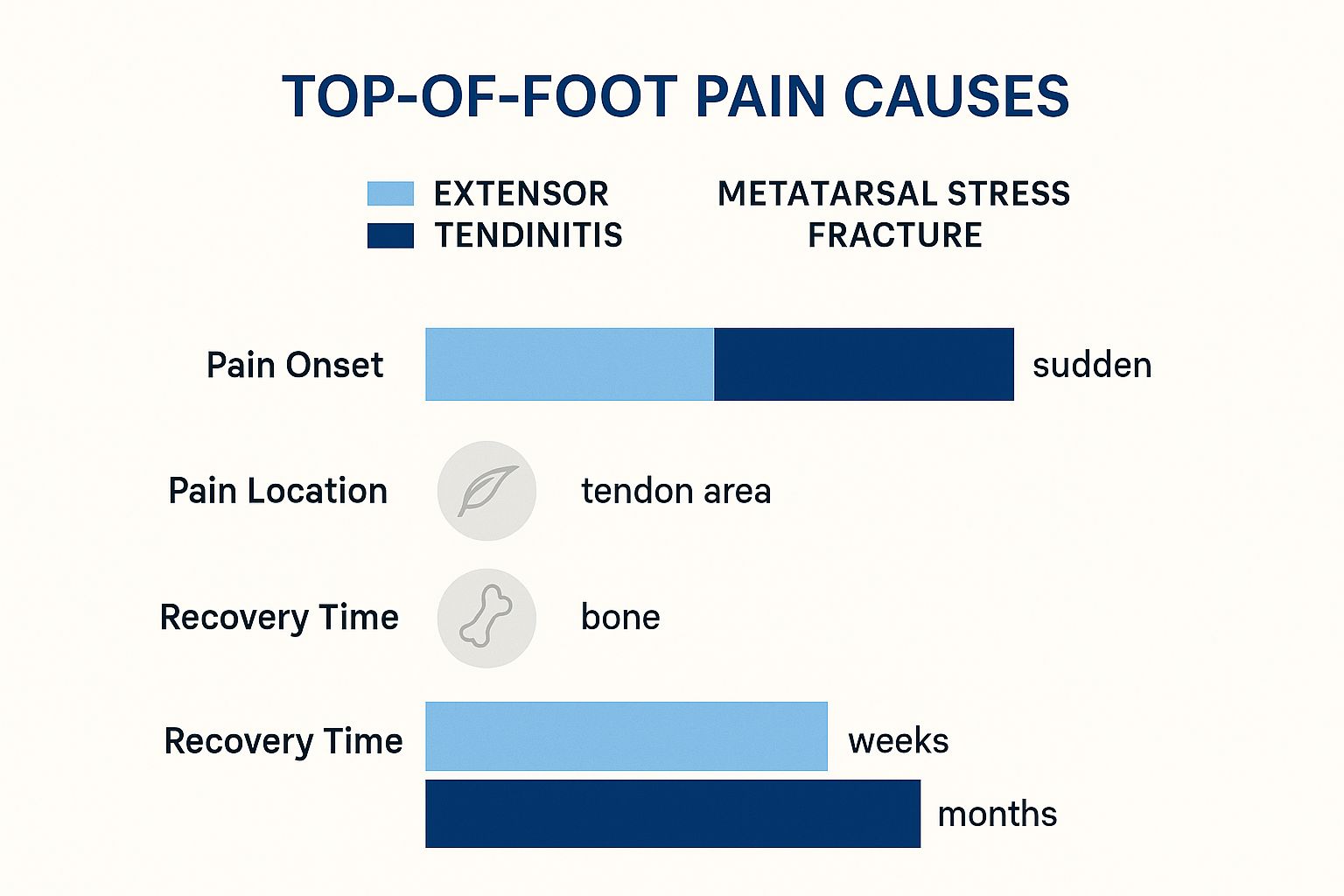
Most top-of-foot problems in runners fall into two camps: soft-tissue overload (extensor tendinitis) or bone stress (metatarsal stress fracture). Both can be painful, but they behave differently — and the management is different. Start with the simple checks below to triage the issue.
The two main suspects
- Extensor Tendinitis: inflammation of the extensor tendons along the top of the foot. Typical triggers: tight shoes / aggressive lacing, sudden mileage or hill increases, or repeated toe-dorsiflexion against resistance (for example repeated uphill sprinting with toes forced into shoe).
- Metatarsal Stress Fracture: a tiny crack in a metatarsal bone from cumulative overload. Presents with sharp, localised pain — often worse with every step, and sometimes worse at rest.
Why runners — especially in Australia — get it
Every stride is an impact. On hot, hard Aussie roads or long coastal pavement runs, that impact adds up. Combine that with aggressive training blocks for local events (Sydney, Melbourne, Gold Coast) and narrow or worn shoes, and you have a perfect setup for overload at the top of the foot.
“Repetitive impact + direct pressure (lacing/shoe) + rapid load increases = tendon overload.” — practical checklist for making training decisions.
Identifying the cause of your foot pain
Play detective before panic. The aim is to determine whether you can manage this at home or whether you need imaging and a clinician.
Prime suspect 1 — Extensor Tendinitis
What to do (trackside): immediately relace to create a pressure-free window over the tender area (skip those eyelets), reduce load (no hills or speed), ice 18 minutes, and swap to zero-impact cross-training (swim/cycle).
Why it works: removing pressure and reducing repetitive dorsiflexion lowers tendon friction and inflammation, while cross-training preserves aerobic fitness without impact.
How to apply (this week): replace your scheduled hill session with 40–60 minutes steady cycling at RPE 5–6 or 30–40 minutes of continuous swimming intervals (10×100m with 20–30s rest). Reassess pain after 7–10 days.
Prime suspect 2 — Metatarsal Stress Fracture
What to do: stop running immediately. See a sports clinician for assessment and imaging (X-ray or MRI). Use crutches or a controlled walking boot if recommended.
Why it works: bone healing needs unloading — continued impact risks conversion to a full fracture and months out.
How to apply: switch to pool running or an aquatic program for fitness maintenance, and plan a conservative 6–8 week non-impact block before a progressive return-to-run protocol as guided by your clinician.
The less common culprits
- Nerve compression / neuroma: burning, tingling, or numbness (feels like a pebble in the shoe). Often shoe-fit related.
- Dorsal ganglion cyst: firm, moveable lump on the top of the foot. Usually assessed by podiatry.
- Arthritic change: deeper, bony ache more likely in older athletes or those with prior injury.

Simple triage checklist (do this now)
- Can you hop on the painful foot without sharp local pain? If no, suspect bone stress and see a clinician.
- Does pain feel worse under the laces and reduce when you alter lacing? If yes, treat as extensor tendinitis (adjust lacing/shoes + reduce load).
- Is there burning/numbness between toes? Check shoe width and consider a podiatry consult for neuroma screening.
Cheat sheet table
| Condition | What it feels like | Common triggers (Aussie context) |
|---|---|---|
| Extensor Tendinitis | Dull, diffuse ache across top of foot; swelling; worse with running and lacing pressure. | Aggressive lacing for long runs; sudden mileage/hill spikes; narrow shoes during humid summer runs. |
| Metatarsal Stress Fracture | Sharp, localised pain; worse during/after runs; worse at rest in advanced cases. | Rapid load increase, low energy availability, worn shoes on hard surfaces. |
| Nerve Compression | Burning/tingling; sense of rubbing/pebble in shoe. | Narrow toe box shoes; swelling during long humid runs. |
Your immediate action plan for pain relief
When it hurts now, act smart. Below is a field-tested, step-by-step plan to reduce pain fast and keep your training productive.
The R.I.C.E. protocol — but smarter
- Rest: stop the aggravating activity (running). Replace with non-impact cardio — 30–60 minutes cycling or 30–40 minutes pool running 2–3 times per week to maintain aerobic base.
- Ice: 18 minutes on the top of the foot, 3–4 times daily for the first 72 hours or until acute pain drops. Use a thin towel to prevent skin damage.
- Compression: light compression if swelling is present — never so tight that it increases pain or numbness.
- Elevation: whenever seated, keep the foot above heart level for 10–15 minutes blocks to reduce fluid build-up.
The easiest win you’re probably missing — lacing
If pain sits under the tongue of your shoe or under the laces, try this immediately:
- Unlace completely down to the eyelets below the painful spot.
- Skip the eyelets directly above the sore area to create a pressure window.
- Lace normally above that point and re-tension to secure the heel.
What to expect: immediate reduction in localized pressure and, in many runners, a noticeable drop in pain within one run or walk.
Gentle mobility & acute drills you can do on the couch
- Alphabet toe-writing: 3 sets of the alphabet with the big toe — moves the ankle through full ROM without impact.
- Towel stretch: 30s × 3 reps — loop a towel around the forefoot and gently pull to dorsiflex; keeps the posterior chain mobile.
- Soft tissue (careful): light massage to surrounding muscle bellies (avoid direct tendon pressure) for 5 minutes once daily.
How to build injury-proof feet for good
Fixing acute pain is phase one. Phase two is building tolerance so you don’t return to the same problem when training load increases.
Strengthen from the ground up — the three moves that matter
Every exercise below follows the UCAN 3-layer test: what to do — why it works — how to apply.
- Towel Curls
What to do: 3 sets of 60 seconds, scrunch the towel with toes; progress to single-leg when comfortable.
Why it works: targets intrinsic foot muscles and arch stabilisers so larger tendons aren’t overloaded.
How to apply: add 3×/week—pair with easy run days or active recovery sessions. - Banded Dorsiflexion
What to do: 3 sets of 12–15 reps seated; loop band over forefoot and dorsiflex against resistance.
Why it works: strengthens the extensor mechanism directly, improving tendon load tolerance.
How to apply: do before runs or as part of warm-ups on key workout days. Progress resistance gradually. - Calf Raises (with a twist)
What to do: slow 3s up / 3s down from step edge, 3 sets of 12–15. Add load when form remains perfect.
Why it works: stronger calf-complex reduces forefoot load by improving ankle rocker and shock absorption.
How to apply: 2–3×/week; include single-leg versions for runners returning from injury.

Get your footwear dialled in
What to do: get a gait analysis at a speciality running store; test shoes with socks and orthotics you’ll use on race day.
Why it works: a shoe that matches your biomechanics reduces shear and pressure on the extensor tendons and evenly distributes load across the metatarsals.
How to apply: track shoe mileage — replace shoes at ~500–800 km depending on your weight, terrain and shoe model. If you’re switching brands or models, run a progressive 2–3 week adaptation (short runs first).
Coach’s note: dead shoes and inconsistent footwear are among the fastest routes to recurrence.
Master your training load — a practical rule
The simplest rule that works: manage weekly load increases. A pragmatic approach is a 10% weekly increase cap on running volume, but apply common sense — reduce when you add speed/hills.
Practical example: if your Base Week is 30 km, keep week-to-week increases to ~3 km (10%). If you add hill sprints or a track session, keep total km the same and replace an easy run instead of adding extra distance.
Fueling for recovery & preventing future injuries
Nutrition is part of the rehab toolbox. If you’re underfuelled, tissue repair slows — tendons and bone don’t get the substrate they need.
Why fuelling matters
Low energy availability impairs connective tissue repair and increases risk of stress injury. Steady energy during long sessions helps maintain form; better form = less abnormal load to the top of the foot.
Practical fuelling recommendations
- Pre-long run: a slow-release UCAN Energy Gel 15–30 minutes before sustained pace work can help keep glucose stable and protect form into the later kilometres. 👉 Shop UCAN Energy Gels
- Post-run (critical window 30–60 mins): target a 3:1 carb:protein ratio to refuel glycogen and support tissue repair — UCAN Energy + Protein is a practical, portable option for this. 👉 Shop UCAN Energy + Protein
- General: ensure daily protein intake (1.2–1.6 g/kg/day for endurance athletes), and maintain consistent calorie availability through heavy training blocks.
When to stop guessing and see a professional
There’s a point where self-management is not enough. Recognise it early and save weeks of frustration.
Non-negotiable red flags (see clinician immediately)
- Pain that’s worse at rest than during activity.
- Pinpoint bone pain that reproduces with single-finger pressure.
- Inability to bear normal weight or significant limp.
- Persistent swelling that doesn’t improve with R.I.C.E.
Physio or podiatrist — who to call first?
Podiatrist: start here if you suspect a bone issue, neuroma or need orthotics / imaging. Physiotherapist: choose this route for biomechanical chain issues (hip weakness, running form) and progressive rehab programming. Both professions often work together for a faster, safer return to running.
FAQ
Can I run through top of foot pain?
Short answer: no. Pain is an alarm. Running through clear signs of tendon overload or possible bone stress risks a longer layoff. Manage early and conservatively.
How long does it take for top of foot pain to heal?
Depends on diagnosis. Mild extensor tendinitis: 1–3 weeks with immediate modification and rehab. More severe tendinitis: 4–6+ weeks. Metatarsal stress fracture: typically 6–8 weeks non-impact, then progressive return (clinician-guided).
Should my running shoes feel tight on top?
No. Shoes should lock the heel and midfoot while leaving room at the front. If you feel direct pressure across the dorsum during runs, address lacing and shoe width immediately.
Can orthotics help with this type of pain?
Yes — when the top-of-foot pain is secondary to a larger biomechanical problem (flat feet, poor arch support, abnormal load distribution). Use a podiatrist to determine if temporary orthoses or custom orthotics are appropriate.
References
[1] Brukner P, Khan K. Clinical Sports Medicine. 5th ed. McGraw Hill, 2017. (tendon overuse and load management principles.)
[2] Nigg BM, et al. Biomechanics and running shoes: the role of loading and cushioning in injury. Br J Sports Med. 2015.
[3] Taunton JE, et al. A retrospective case-control analysis of 2002 runners with stress fractures. Clin J Sport Med. 2002.
[4] University of Melbourne. Centre for Health, Exercise and Sports Medicine — Prevalence and impact of foot pain in the Australian population. 2019.
[5] Sports Medicine Australia. Running Injuries Fact Sheet. 2021.



























Comments are closed